The sympathetic nervous system
Define the sympathetic nervous system
The sympathetic nervous system (SNS) forms part of the autonomic nervous system, controlling many unconscious functions.
It is generally considered a ‘physiological accelerator’.
Outline the origin of the sympathetic nervous system
Higher centres
The SNS receives input from several higher centres in the brainstem and cerebral cortex, such as the:
- limbic system, which includes the hypothalamus, anterior thalamic nuclei, the cingulate gyrus, and the hippocampus
- rostroventrolateral medulla (RVLM), commonly referred to as the vasomotor area
- raphe nuclei
- nucleus tractus solitarius
Preganglionic neurons and the sympathetic chain
The cell bodies of preganglionic nerves are located in the grey matter of the lateral horn of the spinal cord from T1-L2.
From here, the nerve fibres can take 4 paths:
- Synapse at a paravertebral ganglion at the same spinal level
-
each paravertebral ganglion communicates with its corresponding spinal nerve via the white and grey rami communicans
-
preganglionic nerves exit the spinal cord via the ventral root and synapse at the paravertebral ganglion via the white ramus communicans
-
postganglionic nerves exit the paravertebral ganglion via the grey ramus communicans and travel to their target organ via spinal nerves
-
the paravertebral ganglia collectively form the sympathetic chain
-
the sympathetic chain traverses the anterolateral margin of the thoracic vertebral bodies, posterior to the aorta (left) and IVC (right)
-
The white rami are white because they contain myelinated preganglionic nerve fibres. Meanwhile, the grey rami are grey because they contain unmyelinated postganglionic nerve fibres.
Outflow from the sympathetic chain
-
Travel to a different paravertebral ganglion
- preganglionic nerves enter the sympathetic chain via the white ramus communicans but do not synapse right away
- they ascend or descend within the sympathetic chain before synapsing at a paravertebral ganglion at a different spinal level
- postganglionic fibres then exit the sympathetic chain via the grey ramus communicans as usual
-
Pass through the paravertebral ganglia without synapsing
- these preganglionic nerves synapse at prevertebral ganglia such as the:
- coeliac ganglion
- aorticorenal ganglion
- superior mesenteric ganglion
- inferior mesenteric ganglion
- these preganglionic nerves synapse at prevertebral ganglia such as the:
-
Synapse directly on chromaffin cells in the adrenal medulla
- stimulates catecholamine synthesis and secretion
- the adrenal medulla behaves similarly to a postganglionic neuron, releasing catecholamines into the bloodstream instead of directly into a target organ
Describe the course and fibre types
Cervical branches
The cervical ganglia receive input from the T1-7 spinal levels. There are three:
Superior cervical ganglion (C3-4)
- gives rise to the:
- carotid plexus, which surrounds internal carotid artery
- which in turn join parasympathetic fibres to feed the ciliary, pterygopalatine and otic ganglia via cranial nerves 7, 9, 10 and 12
- superior cardiac nerve → superficial and deep cardiac plexuses
- carotid plexus, which surrounds internal carotid artery
Middle cervical ganglion (C6)
- gives rise to the:
- thyroid nerve
- middle cardiac nerve → deep cardiac plexus
Inferior cervical ganglion (C7)
- in 80% of people, is fused with the first thoracic ganglion to form the stellate ganglion
- gives rise to the:
- vertebral artery plexus → brain
- inferior cardiac nerve → deep cardiac plexus
Thoracic branches
Branches from the T1-4 paravertebral ganglia feed into the cardiac, pulmonary and oesophageal plexuses.
Branches from all spinal levels give branches to the aortic plexus.
Thoracic splanchnic nerves
Thoracic splanchnic nerves are preganglionic nerves which originate in the thoracic spine and pierce the diaphragm to synapse on abdominal prevertebral ganglia, to innervate abdominal viscera.
Branches from T5-9 form the greater splanchnic nerve
- which joins the coeliac ganglion → coeliac plexus → coeliac axis and foregut (liver, biliary tree, pancrease, spleen, stomach, proximal duodenum)
- also gives branches to the adrenal medulla
Branches from T10-11 form the lesser splanchnic nerve
- which joins the superior mesenteric and aorticorenal ganglia to innervate the midgut and kidneys
Branches from T12 form the least splanchnic nerve
- which gives branches to the renal plexus
Lumbosacral splanchnic nerves
Although these ganglia are located in the lumbosacral region, the nerves that traverse these ganglia still originate from T1-L2.
Note that pelvic splanchnic nerves originate from S2-4 and only carry parasympathetic fibres.
Lumbar splanchnic nerves arise from lumbar sympathetic ganglia. They feed the inferior mesenteric ganglion, sending branches to the:
- hindgut
- superior hypogastric plexus → iliac vessels and pelvic viscera
Sacral splanchnic nerves arise from sacral sympathetic ganglia. They feed the inferior hypogastric plexus → pelvic viscera (bladder, rectum, uterus, prostate)
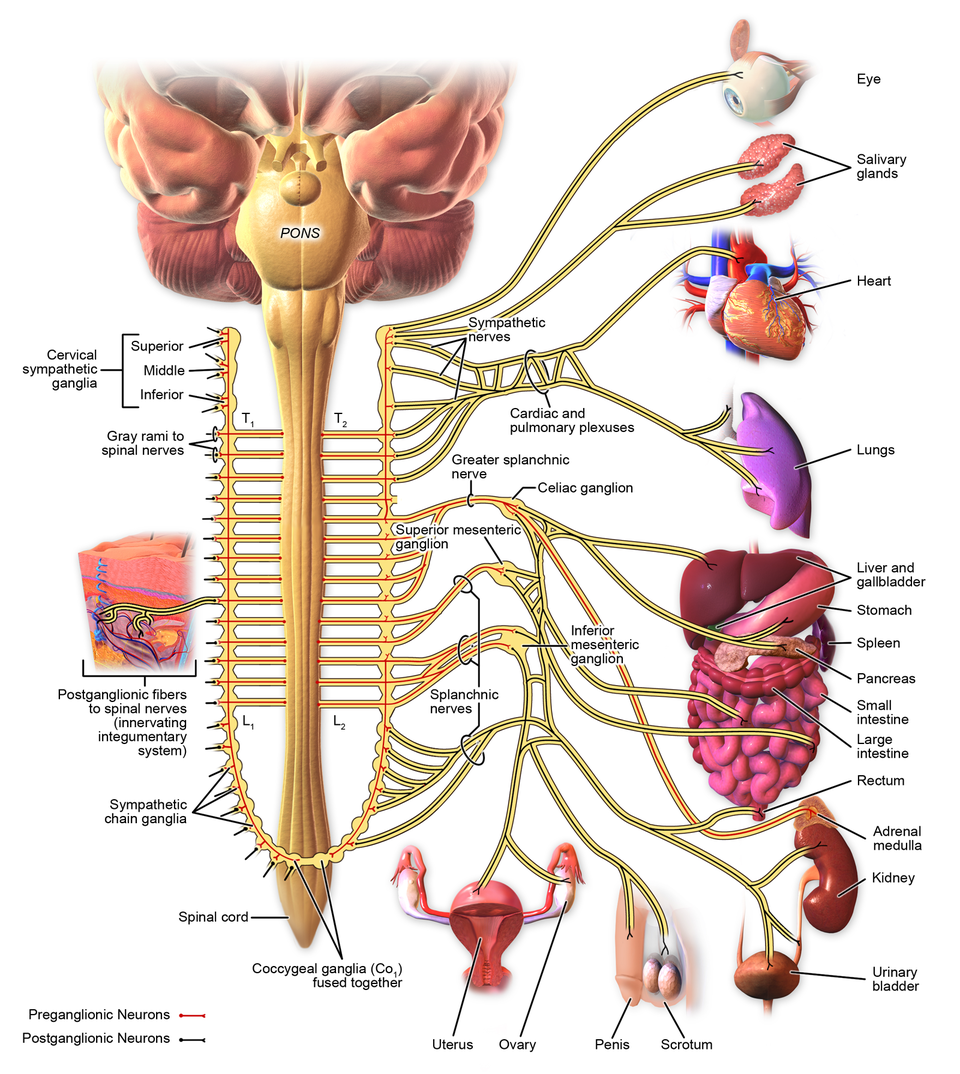
Innervation of the sympathetic chain
By Blausen Medical, licensed under CC-BY 3.0
Nerve fibre types
| Preganglionic | Postganglionic | |
|---|---|---|
| Length | Short | Long |
| Fibre type | Myelinated B-fibres | Unmyelinated C-fibres |
Synapse location | Autonomic ganglia, such as para- and prevertebral ganglia | On target organ |
Neurotransmitter released | Acetylcholine (ACh), which is taken up by type-2 nicotinic receptors (N2 receptors) on post-ganglionic nerves | Predominantly releases noradrenaline, but also adrenaline and dopamine in smaller amounts. Releases ACh in sweat glands and erector pili in skin, important for thermoregulation. |
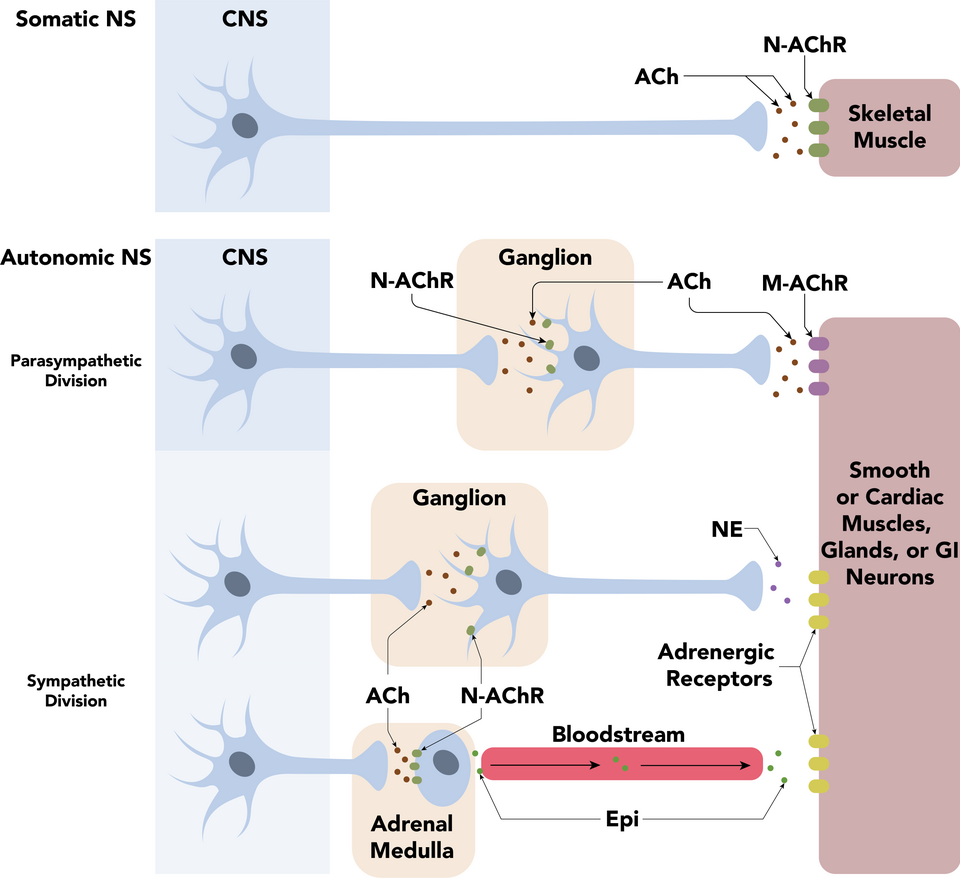
Pre- and post-ganglionic nerve and neurotransmitter types in parasympathetic, sympathetic, and somatic neurones.
By Daniel Walsh and Alan Sved, licensed under CC-BY-SA 4.0
Outline the receptors and neurotransmitters
References
Ellis, Feldman, Harrop-Griffiths, Lawson. Anatomy for anaesthetists, 8th edition. Blackwell Publishing. 2004.

