Acquired immunity
Compare the characteristics of B and T lymphocytes
| T cell | B cell | |
|---|---|---|
| Origin | Both are produced in bone marrow from common lymphoid progenitor stem cells. | |
| Maturation | Migrate to thymus where they are processed. T cells express random unique proteins to form T cell receptors (TCRs). Thymus epithelial cells can produce any protein in the body which are tested for reactivity with TCRs. T cells with TCRs that cannot interact with MHC molecules undergo apoptosis (positive selection). Cells with TCRs that bind to host proteins (self-reactivity) also undergo apoptosis (negative selection). T cells with CD4 glycoproteins can interact with MHC-II molecules and are known as CD4+ or T helper (Th) cells. T cells with CD8 glycoproteins can interact with MHC-I molecules and are known as CD8+ or cytotoxic T (Tc) cells. | Mature in bone marrow. Also express unique proteins in the form of B cell receptors (BCRs) undergoing positive and negative selection in the same way as T cells. |
| Storage | Both are stored in lymphoid tissue | |
| Function | Humoral and cell-based immunity | Humoral immunity only |
| Life span | Memory B and T cells lie dormant and rapidly proliferate on subsequent exposure to the same antigen, causing a rapid immune response, this time with mostly IgG. This is known as active immunity. Non-memory cells will die within 5 days. Memory T cells live for 1-6 months. Memory B cells can live for decades. | |
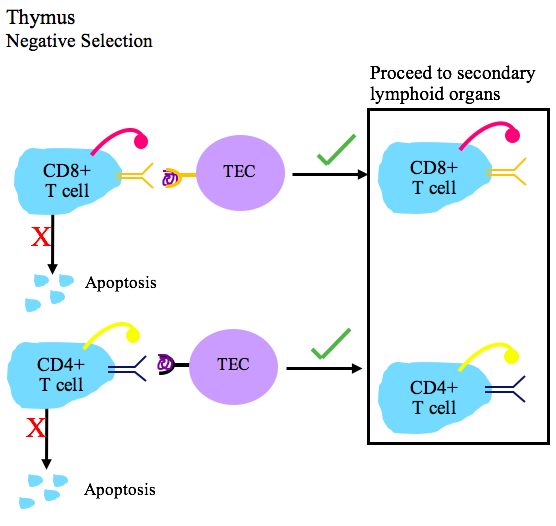
Negative selection of T cells in the thymus. TEC = thymic epithelial cell.
By Immcarle64 CC-BY-SA 4.0 via Wikimedia Commons
Define acquired immunity
A learned response to infection that has memory. It takes up to 5 days to mount an initial response, but can mount a more rapid response on subsequent exposure to a pathogen. It is slower but more specific than the innate immune response.
Describe the acquired immune response
Humoral response
Antigen presentation
Antigen presenting cells (e.g. macrophages, dendritic cells, granulocytes) phagocytose pathogens, breaking them down and presenting them on their cell membrane bound to MHC class II complexes (MHC-II).
They then travel to lymphoid tissue and present the antigen to B cells and T helper (aka Th or CD4+) cells.
Lymphocyte proliferation
Th cells that have T cell receptors matching the antigen replicate to form more Th cells and memory Th cells.
B cells with B cell receptors matching the antigen replicate, with the assistance of Th cells.
B cells then mature into memory B cells and plasma cells, which rapidly secrete antibodies against the antigen. The antibodies are predominantly IgM on initial exposure.
Antibody action
Complement, inactivation, agglutination, opsonisation
Antibodies travel in plasma and bind to pathogens, acting in four main ways:
- Complement activation via the classical pathway
- Inactivation - binding the antigen may inactivate a toxin or an essential part of the microbe
- Agglutination - binding multiple antigens together forms an easier target for leucocytes
- Opsonisation → binding an antigen makes pathogens easier targets for phagocytosis
Repeat exposure
Memory B and T cells lie dormant and rapidly proliferate on subsequent exposure to the same antigen, causing a rapid immune response, this time with mostly IgG. This is known as active immunity.
Non-memory cells will die within 5 days.
Memory B cells can live for decades
Memory T cells live for 1-6 months
Antibodies roam freely in blood where they may bind a pathogen, leading to opsonisation (2a), inactivation (2b) or agglutination (2c). The Fc region of an antibody can bind to phagocytes (3), facilitating the phagocytosis of an opsonised pathogen (4).
By Maher33 CC-BY-SA 4.0 via Wikimedia Commons
Cell-mediated response
All human cells take samples of their intracellular proteins and express them outside their cell membrane on MHC class I complexes (MHC-I).
In the case of intracellular infection (e.g. virus, yeast, tuberculosis, parasite) or abnormal cellular function (malignancy), abnormal proteins are expressed on MHC-I.
Due to the positive and negative selection process described above, cytotoxic T cells (aka Tc or CD8+ cells) have random T cell receptors (TCRs) that only bind to non-host antigens. When the TCR binds the abnormal MHC-I complex, it induces apoptosis in the infected cell.
Tc cells then replicate to form more Tc cells that will identify the same abnormal protein. They travel in plasma to continue fighting the infection. Note that this process does not require antibodies.
Antigen presentation to T helper and cytotoxic T cells via MHC-II and MHC-I respectively.
Describe how immunisation protects against infection
Active immunisation
An inactive fragment of a pathogen is given to the patient, for example by intramuscular injection.
Antigen presenting cells phagocytose the pathogen, breaking it down and presenting it on its MHC-II complex. They present the pathogen fragment to B and T lymphocytes, triggering the acquired immune response and proliferation of memory lymphocytes.
The prolonged lifespan of memory cells means that when a patient is exposed to the actual pathogen in the future, the acquired immune response acts much more rapidly with predominant secretion of IgG antibodies.
Passive immunisation
Antibodies are transferred to a patient. The antibodies facilitate an immune response, however this method does not confer immunity as the acquired immune system does not ‘learn’ the pathogen by creating memory lymphocytes.
Examples:
- administration of HZV IVIg for herpes zoster infection
- passive transfer of maternal antibodies to a developing foetus
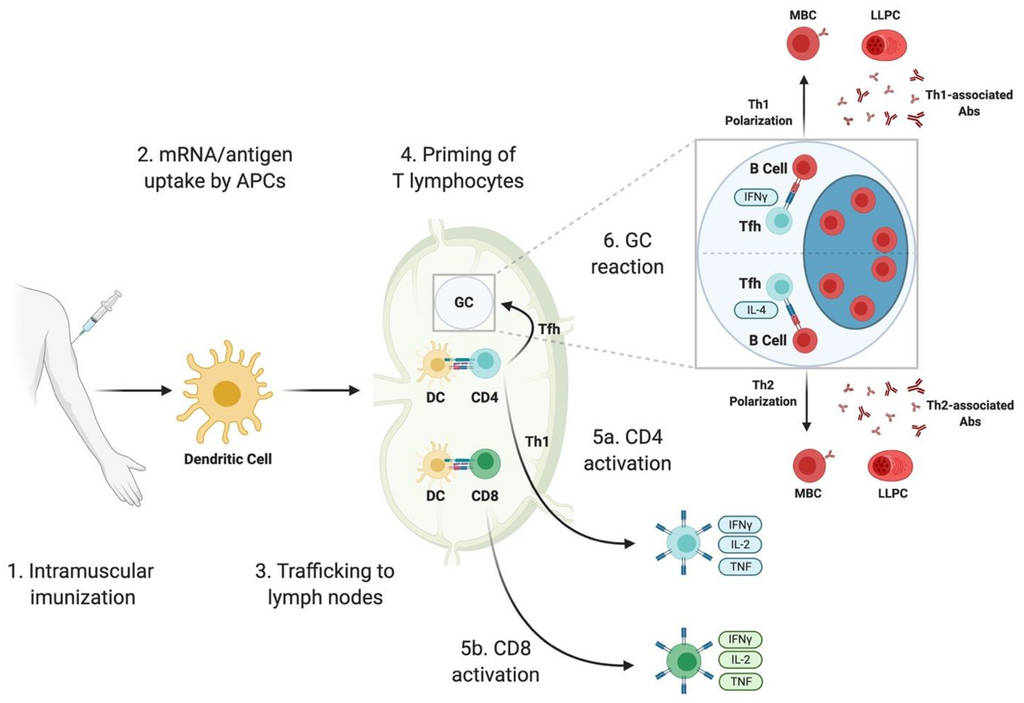
Lymphocyte response to active immunisation.
LLPC = plasma cell. MBC = memory B cell. Tfh = follicular Th cell.By Bettini and Locci CC-BY 4.0 published in Vaccines
Describe the structure of an antibody
The basic unit of an antibody comprises two light chains (red and green) and two heavy chains (blue and yellow) joined by disulfide bonds and arranged in a Y shape.
Heavy chains consist of three constant domains, , and one terminal variable domain, . Light chains consist of one constant domain, , and one terminal variable domain, .
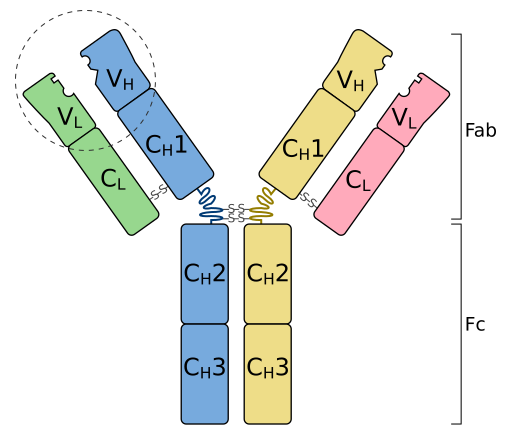
By Tokenzero CC-BY-SA 4.0 via Wikimedia Commons
The Fc region forms the bottom / stem of the Y
- it only contains constant domains and determines the antibody isotype (IgG, IgM, IgA, IgE, IgD)
- it is constant and therefore non-specific, hence its main functions interact with the innate immune system, for example:
- activation of complement
- assists phagocytes to detect opsonised pathogens
- signals for degranulation of granulocytes (e.g. basophils, mast cells)
The Fab region forms the top of each upper limb of the Y
- it contains constant and variable domains
- the variable domains allows different antibodies to bind to different antigens
Antibody isotypes
Different isotypes (IgM, IgG, IgA etc) are distinguished by their overall structure.
- IgM is arranged in a pentameric structure
- IgA is arranged in a dimeric structure
- IgG, IgE and IgD are monomeric. They are distinguished from each other by the structure of their Fc portions.
By Martin Brändli CC-BY-SA 2.5 via Wikimedia Commons

