Innate immunity
Define innate immunity
The innate immune response is a rapid, non-specific response to perceived infection. It does not require prior exposure, and is present since birth. It does not have memory.
Non-immune host defences
Often referred to as physiochemical barriers, these are mechanisms that physically prevent the entry or encourage the excretion of microorganisms from the body.
TIP
Basically every bodily fluid that communicates with the outside world contributes to barrier immunity.
| System | Mechanism |
|---|---|
| Skin | Physical barrier against microbes |
| Saliva | Contains proteolytic enzymes that are toxic to microbes |
| Gastric | Acidic gastric secretions are toxic to many microbes |
| Bile | Outward flow of bile flushes microbes from the biliary tract. The alkaline bile may also be toxic to some microbes. |
| Gut | Peristalsis and defecation flushes out microbes |
| Urine | Outward flow of urine flushes microbes from the urinary tract |
| Respiratory | Mucous catches microbes which are ejected via the mucociliary escalator and cough reflex |
Outline the components of innate immunity
Cellular components
Granulocytes
- Neutrophils - specialised against bacteria and fungi
- Eosinophils - specialised against parasites and helminths
- bind to IgE
- degranulate, releasing major basic protein (kills helminths) and eosinophilic cationic protein (against parasites)
- Basophils
- Mast cells
- found in tissue
- contain a large number of histamine granules which are released on degranulation
- high affinity receptors for IgE
- effect depends on tissue (e.g. bronchoconstriction in lungs and mucous production from mucous membranes)
- Main functions
- phagocytosis of microbes
- degranulation with release of vasodilatory and chemotaxic factors
- antigen presentation to lymphocytes
Macrophages
- Life cycle
- develop as monocytes in bone marrow
- enter circulation and remain for 3 days
- then enter tissue and mature into macrophages or dendritic cells
- NB other types of dendritic cells are derived from their own separate lineage rather than monocytes
- Functions
- phagocytosis of cellular debris
- respiratory burst function - produce oxidative free radicals to kill intracellular pathogens
- breakdown of damaged tissues/cells
- antigen presentation - process and present foreign pathogens to B and T cells on their MHC-II complexes
- Specialised against
- intracellular pathogen (e.g. Listeria)
- mycobacteria
- fungi
- parasites
Dendritic cells
- present in many tissues
- activate on exposure to pathogens and act as an antigen presenting cell
Natural killer cells
- granular secretory lymphoid cells with T lymphocyte morphology
- found in blood, spleen, liver
- half life ~ 1 week
- specialised against
- tumour cells
- virus-infected cell
- fungi
- parasites
- 2 mechanisms for cytotoxicity
- antibody-dependent cellular cytotoxicity (ADCC)
- posess immunoglobulin receptors (FcR) which bind antibody coated targets
- release perforins and granzymes, leading to lysis of the target cell
- via MHC-I
- posess receptors for MHC-I
- → detect cells expressing low levels of MHC-I, such as virus infected or cancerous cells
- → insertion of perforins into target cell
- → delivery of cytotoxic enzymes and cell lysis
- antibody-dependent cellular cytotoxicity (ADCC)
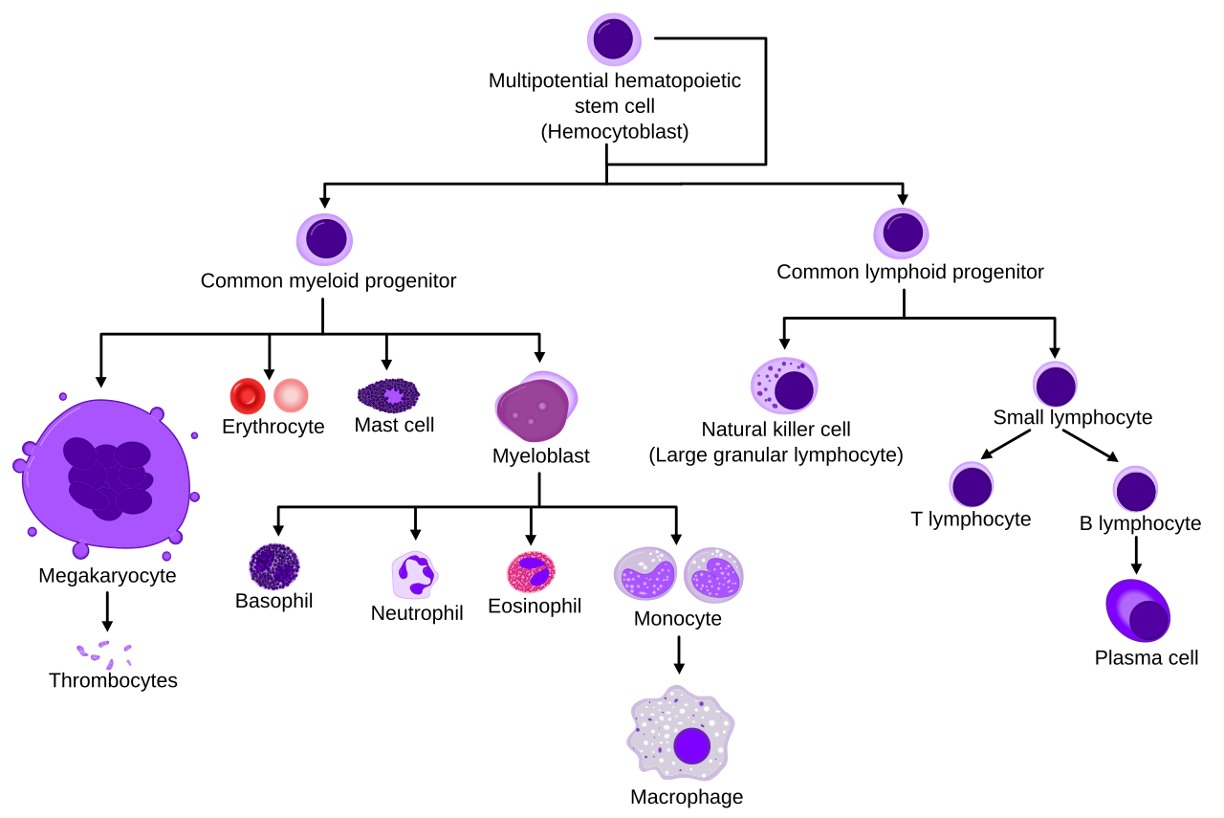
By A. Rad and M. Häggström CC-BY-SA 3.0 via Wikimedia Commons
Humoral components
Lysozymes
- proteolytic enzymes present in mucosal surfaces and many phagocytes
- they break down bonds in bacterial cell wall peptidoglycans → cell lysis
- in phagocytes, this facilitates the presentation of bacterial fragments on MHC-II complexes
- they also play a role in both potentiating and suppressing pro-inflammatory cytokines
Acute phase proteins
- mostly synthesised in the liver, stimulated by cytokines (e.g. IL-6, TNF-alpha)
- serve various immune functions such as opsonisation and regulation of inflammatory mediators
- e.g. CRP, fibronectin, a1-antitrypsin, a2-macroglobulin
- CRP binds bacterial cell walls and activates classical complement pathway
- fibronectin binds bacteria to macrophages/monocytes, enhancing their phagocytic activity
- >25 plasma glycoproteins that are mostly made by the liver, the most important of which are C1-9
- they are activated in cascade and serve as important signalling molecules with intrinsic antimicrobial activity
ON THIS PAGE

