Hypersensitivity and anaphylaxis
Classify hypersensitivity reactions
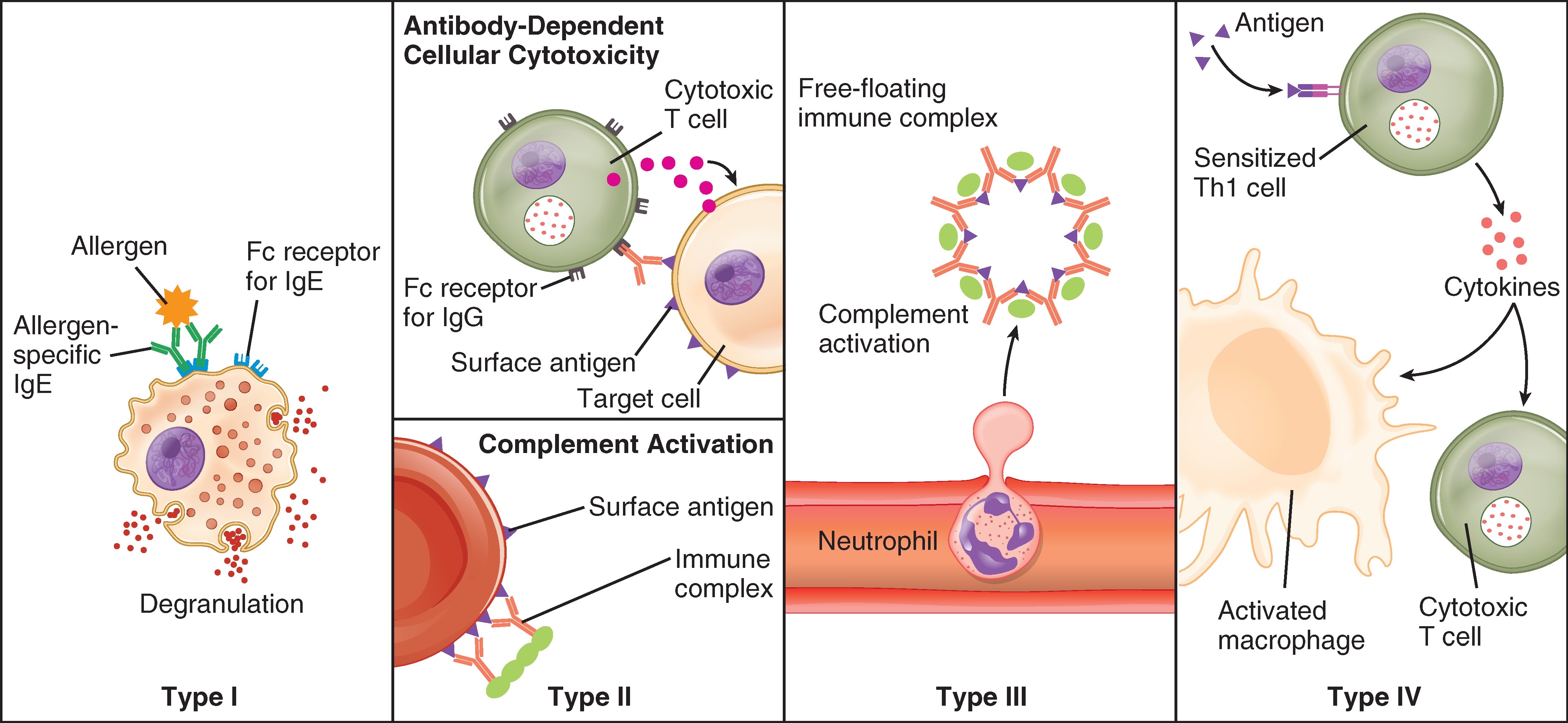
- Allergic (aka immediate hypersensitivity)
- Cytotoxic (aka antibody mediated)
- Immune-complex mediated
- Delayed (aka cell mediated)
Note that both type II and type III are in face antibody mediated, but the Ag-Ab complexes are membrane-bound in type II and 'loose' (soluble) in type III.
Type I - Allergic (immediate)
Onset within minutes if already sensitised
Physiology
-
Initial sensitisation
- detection of an antigen triggers lymphocytes to secrete IgE, which are taken up by basophils (in plasma) or mast cells (in tissue)
-
Subsequent exposures
- the antigen binds to membrane-bound IgE on basophils and mast cells, forming cross-links
- these cells degranulate, releasing various vasodilatory, inflammatory and chemotactic mediators:
- histamine
- tryptase
- leukotrienes
- prostaglandins
- SRSA (slow releasing substance of anaphylaxis)
- eosinophilic chemotactic factor (ECFA)
- neutrophilic chemotactic factor (NCF)
-
Effects
- vasodilation with increased vascular permeability / capillary leak
- → hypotension, oedema (e.g. laryngeal)
- eosinophil/neutrophil infiltration → contributing to immune response
- bronchospasm
- urticarial rash
- vasodilation with increased vascular permeability / capillary leak
-
Regulatory role of eosinophils
- eosinophils play a complex role in anaphylaxis, both contributing to and regulating inflammation
- they inhibit some inflammatory mediators (e.g. SRSA) and destroy antibody-antigen complexes, which may limit the severity of inflammation
Examples
- anaphylaxis
- asthma
- allergy
- atopy
Type II - Cytotoxic (membrane-bound Ag-Ab complex)
Onset within hours to days.
Physiology
- IgM or IgG binds to antigens on cell membrane
- the cell-bound antigen-antibody complex triggers an immune response:
- antibody opsonises the cell, leading to phagocytosis of the cell
- complement is activated via the classical pathway → cell lysis
- neutrophils bind the Ag-Ab complex → degranulate, releasing inflammatory mediators
- NK cells bind the Ag-Ab complex → induce apoptosis (antibody dependent cellular cytotoxicity)
- macrophages activated → phagocytosis and cytokine release
Examples
- acute or delayed haemolytic transfusion reaction
- autoimmune haemolytic anaemia
- haemolytic disease of the newborn (Rh)
- myasthenia gravis
Type III - Immune complex mediated (soluble Ag-Ab complex)
Onset within hours to weeks, typically 3-4 days.
Physiology
- antigen-antibody complexes form either in tissue, causing local effects, or in blood where they deposit in vessel walls causing systemic effects
- activates complement via classical pathway and recruits granulocytes and macrophages as seen in type II hypersensitivity
Examples
- SLE - ANA and nuclear antigens bind in serum and lodge in blood vessels → vasculitis
- IgA nephropathy - complexes lodge in glomeruli → glomerulonephritis
Type IV - Delayed (cell-mediated)
Onset in 2 to 3 days
Physiology
- an antigen presenting cell presents an antigen to a Th1 cell → T-cell proliferation
- repeat presentation causes T-cell activation and cytokine release
- → activates macrophages
- → may cause granuloma formation with fibrosis and calcification
- it is a delayed response due to the time required for T-cell replication and activation
Examples
- TB
- sarcoidosis
- granulomatosis with polyangiitis (GPA)
- poison ivy / contact dermatitis
- SJS/TENS
OpenStax College CC BY 3.0 via Wikimedia Commons, cropped
Anaphylaxis
Anaphylaxis is an acute, severe abnormal immune response affecting multiple systems with at least one of skin, respiratory or cardiovascular symptoms.
Anaphylaxis is a type 1 hypersensitivity reaction.
Describe the drug treatment of anaphylaxis
Supportive
O2
- to treat hypoxia as a result of bronchospasm, airway obstruction, or haemodynamic compromise
- avoid hyperoxic hypoventilation
IV fluids
- vasodilation causes distributive shock
- IV fluid supports blood volume
Immediate management
Adrenaline
- onset: <2min
- route: IM 500mcg initial dose, IV infusion, nebulised
- mechanism of action
- α1 agonism
- Gq-coupled receptor
- → activates PLC → ↑IP3/DAG → ↑ intracellular Ca
- → vasoconstriction
- → decreases oedema (e.g. airway)
- → supports blood pressure
- β agonism
- Gs-coupled receptor
- → activates adenylate cyclise → ↑cAMP → activates PKA → several downstream effects
- β1 effect
- ↑ Ca → inotropy to support haemodynamics
- β2 effect
- acts on mast cells to inhibit release of histamine and SRSA
- inhibits MLCK and indirectly activates MLCP → bronchodilation
- β1 effect
- α1 agonism
Salbutamol (β2 agonist)
- inhaled/nebulised salbutamol may be used as an adjunct for additional β2 effect
Auxiliary management
Second generation antihistamine (anti-H1)
- antagonist at H1 receptors e.g. cetirizine
- does not relieve shock or airway obstruction
Corticosteroids
- e.g. hydrocortisone IV or prednisolone PO
- onset ~1h (hydrocortisone) or 1-2h (prednisolone)
- not part of routine management and should not replace adrenaline
- mechanism of action
- binds to cytoplasmic glucocorticoid receptors
- these undergo conformational change and are actively transported into the nucleus
- there they bind to transcription factors, regulating RNA synthesis
- ↓ synthesis of proinflammatory cytokines and inflammatory mediators (e.g. prostaglandins, platelet activating factor, leukotrienes, COX-2)
- inhibits function of virtually all immune cell lineages
- ↑ number and activation of adrenergic receptors
- effects
- ↓ vascular permeability → ↓ oedema, secretions
- ↓ inflammatory response → ↓ vasodilation/bronchoconstriction
- supports haemodynamics via adrenergic effects

